AI detects hidden tumors physicians missed
- Jul 3, 2025
- 3 min read
Updated: Jul 11, 2025

The impactful testimony of Dianne Covey, a 69-year-old woman from Surrey. Dianne used to be skeptical about AI, but her life changed drastically when a routine chest X-ray revealed nothing, despite her persistent cough. Fortunately, that same day, Royal Surrey County Hospital was installing a revolutionary AI tool, Annalise.ai, which re-analyzed her scan and immediately detected an anomaly. This led to an emergency CT scan and a diagnosis of stage one lung cancer, which was not visible to the naked eye and would have taken six months for a radiologist to detect. Thanks to this early AI-assisted detection, Dianne was able to have surgery to completely remove the cancer without the need for chemotherapy or radiotherapy, and she has fully recovered. She states: "Artificial intelligence saved my life."
Dianne's story is not an isolated case. The UK is witnessing a wave of AI tools for detecting, diagnosing, and treating cancer in the NHS, a result of concerted government investment. In October 2023, the NHS announced an investment of £21 million in AI tools for lung cancer diagnosis, and in May 2024, £15.5 million was allocated to implementing AI to reduce waiting times in radiography departments.
But how is AI actually used in this context? Experts clarify that AI does not replace doctors, but acts as a "second pair of eyes" to help them work better. Its primary function is to reduce the workload of overburdened healthcare staff. AI is exceptional at pattern recognition, trained with thousands of scans to identify anomalies that the human eye might overlook.
Mike Jones, a radiologist at the Royal Surrey NHS Foundation Trust, explains that traditionally, hundreds of X-rays were read in chronological order, delaying urgent cases. With AI, each X-ray is analyzed immediately after being taken, flagging critical findings to prioritize them on the radiologist's worklist. This prioritization system is crucial, as it helps mitigate human errors and accelerates diagnosis, which can be vital for the patient's prognosis.
In addition to Annalise.ai, which has already been adopted by more than 45 NHS trusts, other AI tools are making a difference:
Pi, developed by Lucida Medical, analyzes MRI scans to help diagnose prostate cancer, differentiating between low- and high-risk cases to avoid unnecessary and costly biopsies.
DERM, an AI system that allows doctors to triage suspected skin cancer referrals using a smartphone, is used in 21 NHS trusts. With a photo of a suspicious lesion, the system evaluates with 99% accuracy in minutes. This is especially useful given that one in four consultant dermatologist positions in the UK are unfilled.
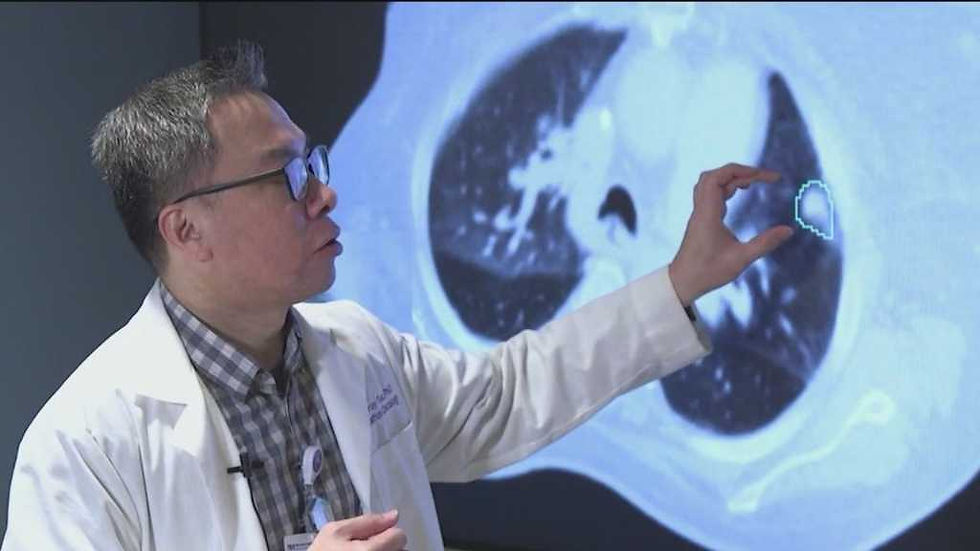
In the field of radiotherapy, iSeg, a tool developed by Northwestern Medicine scientists, is revolutionizing lung tumor segmentation. This 3D deep learning system is the first to delineate tumors as they move with each breath, a critical factor in treatment. iSeg matches experts and identifies areas of cancer that some doctors might overlook, linked to worse outcomes if left untreated.
Qure.ai, another AI tool, is being studied at University Hospitals to detect lung cancer nodules that are almost impossible to see in early stages. Trained with millions of X-rays, Qure.ai can identify "super-hidden" lesions, with the hope of diagnosing cancer in stages one or two, which could increase survival rates to 60-70%.
Despite these advances, initial skepticism exists among patients and medical staff. Furthermore, significant risks have been identified, such as bias in training data that could exacerbate existing health outcome inequalities, especially in ethnic minorities. The need for more modern MRI machines for AI to function correctly also poses challenges in hospitals with older equipment. Additionally, AI is not infallible and there can be false negatives, although the combination of human and AI interpretations significantly improves results. Another risk is that patients rely on less reliable forms of AI, such as ChatGPT, for treatment decisions.
However, the benefits, such as early detection and reduced workload, outweigh the risks for many. AI is seen as a complementary tool that promises to revolutionize and improve a highly demanded healthcare service. As Claire Maymon, another patient who benefited from DERM, concludes: "AI has arrived just in time to help me and my generation."










Comments